#endcancer
#Cancer #Immunotherapy and Breaking Immune Tolerance
http://t.co/Lt4cqntj4b
Abstract
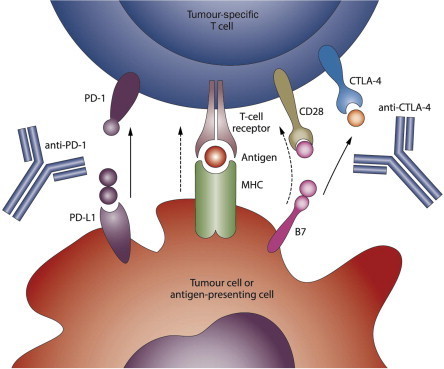
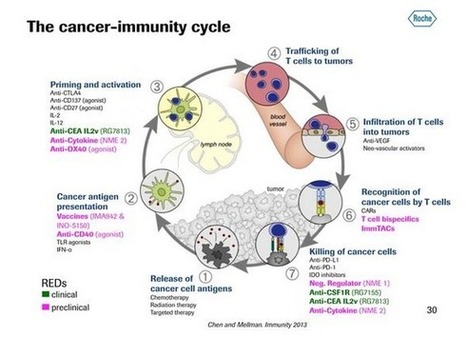
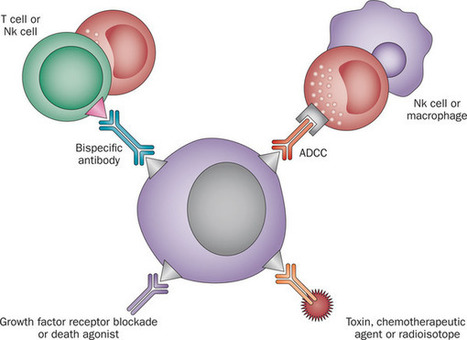
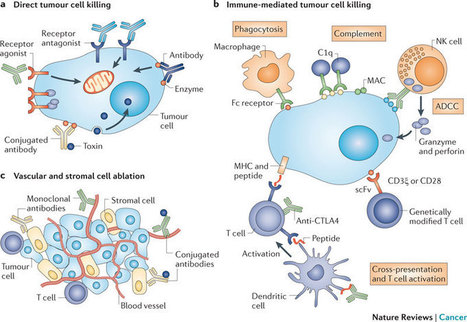
Cancer immunotherapy has proven to be challenging as it depends on overcoming multiple mechanisms that mediate immune tolerance to self-antigens. A growing understanding of immune tolerance has been the foundation for new approaches to cancer immunotherapy. Adoptive transfer of immune effectors such as antitumor mAb and chimeric antigen receptor T cells bypasses many of the mechanisms involved in immune tolerance by allowing for expansion of tumor-specific effectors ex vivo. Vaccination with whole tumor cells, protein, peptide, or dendritic cells has proven challenging, yet may be more useful when combined with other cancer immunotherapeutic strategies. Immunomodulatory approaches to cancer immunotherapy include treatment with agents that enhance and maintain T-cell activation. Recent advances in the use of checkpoint blockade to block negative signals and to maintain the antitumor response are particularly exciting. With our growing knowledge of immune tolerance and ways to overcome it, combination treatments are being developed, tested, and have particular promise. One example is in situimmunization that is designed to break tolerance within the tumor microenvironment. Progress in all these areas is continuing based on clear evidence that cancer immunotherapy designed to overcome immune tolerance can be useful for a growing number of patients with cancer. Cancer Res; 75(1); 5–10. ©2014 AACR.
Via Krishan Maggon



 Your new post is loading...
Your new post is loading...








Published OnlineFirst December 18, 2014; doi: 10.1158/0008-5472. CAN-14-2538 Cancer Res January 1, 2015 75; 5Cancer Immunotherapy and Breaking Immune Tolerance: New Approaches to an Old ChallengeAmani Makkouk1 and George J. Weiner1,2,*
+Author Affiliations
1Interdisciplinary Graduate Program in Immunology, University of Iowa, Iowa City, Iowa.2Holden Comprehensive Cancer Center and Department of Internal Medicine, University of Iowa, Iowa City, Iowa.↵*Corresponding Author:
George Weiner, Holden Comprehensive Cancer Center at The University of Iowa, 5970Z JPP, University of Iowa, Iowa City, IA 52242. Phone: 319-353-8620; Fax: 319-353-8988; E-mail: george-weiner@uiowa.edu